This issue brief addresses the topic of global payments for surgeons under the Medicare physician fee schedule (PFS): what they are, how they work (or don’t work) and why CMS seems so intent on doing away with them. For a great backgrounder on the PFS, as well as some really thoughtful ideas about Medicare payment reform, check out this recent report from HMA and this issue brief from KFF.
What is the Surgical Global
According to coding and billing guidance published by the Centers for Medicare and Medicaid Services (CMS), The global surgical package, “includes all necessary services normally provided by a physician (or members of the same group with the same specialty) before, during, and after a procedure.[1]” There are three types of global surgical packages
- 0-Day Post-Operative Period (endoscopies and some minor procedures)
- No pre-operative period
- No post-operative days
- Generally, a visit on procedure day isn’t payable as a separate service
- 10-Day Post-Operative Period (other minor procedures)
- No pre-operative period
- Generally, a visit on procedure day isn’t payable as a separate service
- Total global period is 11 days; count the surgery day and the 10 days immediately following the surgery day
- 90-day Post-Operative Period (major procedures)
- 1-day pre-operative included
- Generally, procedure day isn’t separately payable
- Total global period is 92 days; count 1 day before surgery, the day of surgery, and the 90 days immediately following the surgery day
Note that Medicare physicians in the same group practice, with the same specialty, must bill and accept payment as though they are a single physician.
Every global surgery (e.g., cataract surgery, quadruple bypass, etc.) has been defined in the American Medical Association (AMA) Current Procedural Terminology (CPT). CPT represents a set of codes used for medical coding and billing as well as communication across the healthcare system. CPT doesn’t just include procedures. It also includes healthcare services like doctor’s office visits are called evaluation and management (E/M) services. E/M codes “represent services by a physician (or other health care professional) in which the provider is either evaluating or managing a patient’s health[2].” . Each global period accounts for a certain number of these E/M visits to occur in the post operative period so that the surgeon can monitor the patient’s recovery. In the CY 2025 PFS proposed rule, CMS specifies that 10- and 90-day globals include “post-operative evaluation and management (E/M) visits and discharge services provided during specified post-operative periods[3].”
While surgeons and other proceduralists are not likely to bill Medicare directly for E/M services, the post-op visits that are included as a part of the global surgical package are actually E/M visits. It therefore follows that these post-op visits, if taken independent of the global, would have a value that should be equal to a certain type of E/M visit
The Issue
In 2009, the Office of the Inspector General (OIG) for the Department of Health and Human Services (HHS) published a report claiming that Medicare paid $97.6 million for E/M services that were included in eye global surgery fees but not provided during the global surgery periods in calendar year 2005.[4] In 2012, it was orthopaedic surgeons’ turn. The OIG estimated that Medicare paid a net $49 million for E/M services that were included in musculoskeletal global surgery fees but not provided during the global surgery periods in 2007. The Medicare Payment Advisory Commission, an independent Congressional agency established in 1997 to advise Congress on issues affecting the Medicare program has expressed similar concerns (including in this 2018 report to Congress) over the rate of reimbursement for specialty care and about the validity of 10- and 90-day global surgery codes[5].
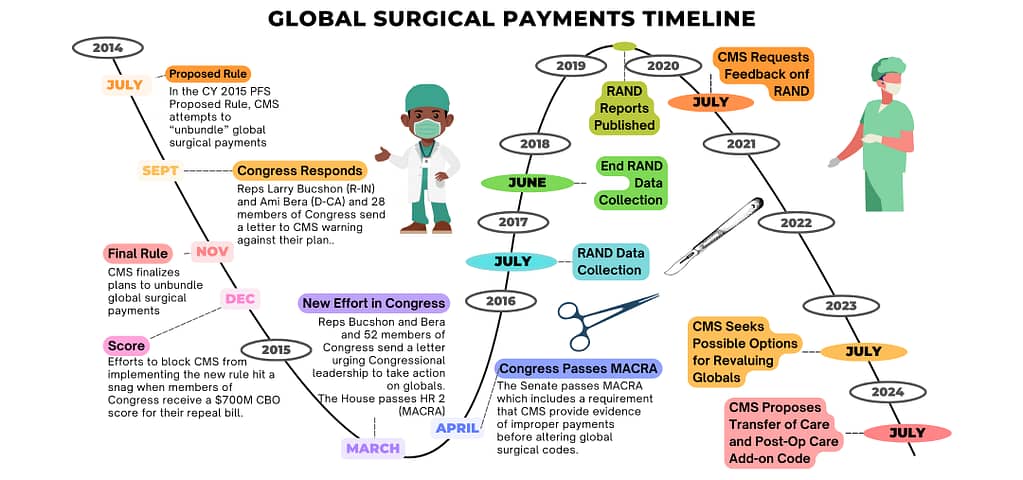
In 2014 CMS responded to these concerns by proposing to completely deconstruct global surgical payments and requiring surgeons to bill separately for each service provided. Surgeons argued that unbundling the global would increase administrative burden and ultimately compromise patient care. A timeline of events is included at Appendix A showing that Congress ultimately blocked CMS from unbundling global payments until CMS could provide data demonstrating that the post-op visits included in the bundles were not taking place.
Deterred but not defeated, CMS contracted with the RAND Corporation “to (1) analyze patterns of the number of post-operative visits provided during the global period, (2) field a practitioner survey designed to capture the level of post-operative visits that take place during the global period, and (3) describe how the newly collected claims-based data on the number of post-operative visits could be used to adjust valuation for procedures with 10- and 90-day global periods[6].” RAND commenced with data collection which included mandatory E/M reporting by select surgeons in nine states. From July 1, 2017 to June 30, 2018, CMS required groups with ten or more practitioners in nine states (Florida, Kentucky, Louisiana, Nevada, New Jersey, North Dakota, Ohio, Oregon, and Rhode Island) to record code 99024 to reflect any post-operative visit performed during the global period for 293 common procedure codes. By July 2019 the RAND Corporation had published three reports:
- Claims-Based Reporting of Post-Operative Visits for Procedures with 10- or 90-Day Global Periods: Final Report[7]
- Using Claims-Based Estimates of Post-Operative Visits to Revalue Procedures with 10- and 90-Day Global Periods[8], and
- Survey-Based Reporting of Post-Operative Visits for Select Procedures with 10- or 90-Day Global Periods: Final Report[9].
CMS invited comments on these reports in the calendar year 2020 Physician Fee Schedule Proposed Rule and several organizations expressed concerns about the content of the reports including:
- There was a lack of awareness about the RAND survey and mandated reporting in 9 states and collection of 99024 contradicts specialty society coding education so even those surgeons who knew to participate may have been confused.
- The mandate to report 99024 layered new administrative burdens on practices which may have impacted participation. However, RAND also excluded small practices from the data collection requirement which may have helped to alleviate the administrative burden but likely skewed the results.
- There was significant confusion about which physicians were required to report and the duration of the reporting period.
- Billing clearinghouses typically don’t recognize zero charge bills. Some practices encountered difficulties reporting 99024, as this code lacks value ($0.00), so attempts to report the code in many practices and EHR systems were blocked by the software.
In another example of what surgeons deemed to be faulty methodology, raw data collected by RAND showed that thoracic surgeons performed 276 10-day global procedures with only forty 99024 codes reported and cardiac surgeons performed 144 10-day global procedures with only twenty-five 99024 codes reported. This would be a damning result if accurate but surgeons pointed out that there were no 10-day global procedures on the list of codes for mandatory reporting that would typically be performed by cardiac or thoracic surgeons. Therefore, these data either pointed to a flaw in the data collection methodology or the assumptions that RAND had made regarding whether or not their data was generalizable.
RAND researchers responded to those criticisms in a report that was initially published in 2019 and updated in 2021 to include a clarification on RAND’s definition of clean procedures or “billed procedures with a single procedure (one billed unit of service) that does not occur within the global period of another procedure with a 10- or 90-day global period[10]. Confusion over this terminology originally led some to question whether RAND understood coding and billing practices. For example, a person undergoing a coronary artery bypass graft procedure (CABG) hardly ever has surgery on just one vessel. However, the procedure is coded as a single vessel CABG with additional vessels. There was concern that, based on their own flawed definition, RAND would have excluded from their analyses one of the most common procedures performed on Medicare beneficiaries, a multi-vessel CABG.
Ultimately, CMS declined to make further changes to global surgical codes, except in 2021 when CMS updated the value of stand along E/M codes but declined to apply that same increase to the value of the E/M codes included in the globals. CMS justified this action citing the MACRA provision that blocked them from making changes to global surgical reimbursement without evidence. Surgeons countered, arguing that that changing the value of E/M and not globals changed the relative value of those codes, making CMS in violation of the MACRA mandate. Surgeons also said that that CMS had disrupted the relativity of the fee schedule[11] and actually violating the law[12] by paying different types of physicians differently for performing the same service. Ultimately, the surgeons were unsuccessful in their efforts and the value of the E/M visits as a component of the surgical global remain unchanged.
Adding insult to injury, surgeons not only did not get a pay boost like primary care doctors but, because of budget neutrality rules, they had to pay for the primary care providers’ raise. Ultimately, this change did not have a huge impact on either the surgeons or in-office physicians because the primary care pay bump still wasn’t enough to account for all the fee schedule cuts scheduled for that year (conversion factor, sequestration, inflation, and more, as well as loss of physician income due to the COVID pandemic) so Congress stepped in to soften the blow.
What’s New
There has been considerable activity around global surgical reimbursement, recently. OIG has recently announced a new review of post-operative services provided in the global surgery period[13]. The CMS website on Global Surgery Data collection also has relatively new data and reports available from 2019 data collection. In August of last year, RAND released a publication, Claims-Based Reporting of Post-Operative Visits for Procedures with 10- or 90-Day Global Periods: Updated Results Using Calendar Year 2019 Data. In their new publication, RAND recommends that CMS consider one or more of the following polity options:
- Revalue 10-day global procedures as 0-day global procedures
- Revalue 90-day global procedures using the number of post-operative visits reported
- Obtain new recommendations from the AMA Relative Value Update Committee (AMA-RUC) the AMA body that makes recommendations to CMS on the relative value of each medical code in the healthcare system.
Most notably, in the CY 2025 PFS proposed rule, CMS has proposed to
- Revise the transfer of care policy for global packages to address instances where one practitioner furnishes the surgical procedure and another practitioner furnishes related post-operative E/M visits during the global period, and
- Develop a new add-on code that would account for resources involved in postoperative care provided by a practitioner who did not furnish the surgical procedure[14].
CMS is transparent is suggesting that both of these policies are aimed at helping them to collect better data on how care is being provided during the global surgical period. With this information, CMS can press forward with its plan to re-value global surgical services. Both changes are described in more detail below.
Transfer of Care
During the global period, if a practitioner other than the proceduralist (or a practitioner in the same group practice as the proceduralist) provides patient care, that practitioner can bill separately for an E/M visit for services they furnish, except where a formal transfer of care modifier applies.[15] Currently, any physician billing with any one of these modifiers must also have a documented, formal transfer of care agreement. The transfer of care modifiers describe the different portions of the global surgical package that could be provided by different practitioners:
- Modifier -54 Surgical Care Only
- Modifier -55 Post-operative Management Only
- Modifier -56 Pre-operative Management Only
However, CMS notes that there could be a number of reasons why incidences of transfer of care were not accurately documented. Therefore, this year they are proposing to require the use of the appropriate transfer of care modifier for all 90-day global surgical packages in any case when a practitioner plans to furnish only a portion of a global package.
CMS is also seeking feedback on how to accurately value the three portions of the global period that are designated by the modifiers. Specifically, CMS requests, a “procedure-specific, data-driven method for assigning shares to portions of the global package payment[16].” In its impact estimates, CMS notes that they expect that, with these new rules in place, the -54 modifier will be used in 20% of surgeries.[17]
Post-operative Care Services Add-on Code
In recognizing that the provider who sees the patient in the post-operative period may not always be the practitioner who performed the surgery, CMS has proposed to create an add-on code to be billed with an office/outpatient E/M visit for follow-up care. This add-on code will accommodate the added level of complexity involved with a provider (who is not of the same practice or specialty) assuming responsibility for patient care after the surgery has taken place. CMS notes that the post-operative practitioner may not have been a part of the treatment planning or may not even have access to the patient’s medical records. CMS states that, “instituting an add-on code to capture the time and intensity of post-operative work absent a formal transfer of care, would be an essential step in recognizing how the services are currently furnished and make meaningful progress toward ‘right-sizing’ the structure of the global packages[18].” The add-on code description is as follows:
Post-operative follow-up visit complexity inherent to evaluation and management services addressing surgical procedure(s), provided by a physician or qualified health care professional who is not the practitioner who performed the procedure (or in the same group practice), and is of a different specialty than the practitioner who performed the procedure, within the 090-day global period of the procedure(s), once per 090-day global period, when there has not been a formal transfer of care and requires the following required elements, when possible and applicable:
- Reading available surgical note to understand the relative success of the procedure, the anatomy that was affected, and potential complications that could have arisen due to the unique circumstances of the patient’s operation.
- Research the procedure to determine expected post-operative course and potential complications (in the case of doing a post-op for a procedure outside the specialty).
- Evaluate and physically examine the patient to determine whether the post-operative course is progressing appropriately.
- Communicate with the practitioner who performed the procedure if any questions or concerns arise. (List separately in addition to office/outpatient evaluation and management visit, new or established)).[19]
CMS anticipates that this add-on code will be used on 40,000 total claims in CY 2025.[20]
[1] https://www.cms.gov/files/document/mln907166-global-surgery-booklet.pdf
[2] https://www.ama-assn.org/topics/evaluation-and-management-em-coding
[3] Medicare and Medicaid Programs; CY 2025 Payment Policies under the Physician Fee Schedule and Other Changes to Part B Payment and Coverage Policies; Medicare Shared Savings Program Requirements; Medicare Prescription Drug Inflation Rebate Program (CMS-1807-P); Posted by the Centers for Medicare&Medicaid Services on Jul 10, 2024. p. 337. https://www.regulations.gov/document/CMS-2024-0256-0001
[4] https://oig.hhs.gov/reports-and-publications/all-reports-and-publications/nationwide-review-of-evaluation-and-management-services-included-in-eye-and-ocular-adnexa-global-surgery-fees-for-calendar-year-2005/
[5] https://www.medpac.gov/wp-content/uploads/import_data/scrape_files/docs/default-source/reports/jun18_medpacreporttocongress_rev_nov2019_note_sec.pdf. Chapter 3: Rebalancing Medicare’s physician fee schedule toward ambulatory evaluation and management services.
[6] https://www.rand.org/content/dam/rand/pubs/research_reports/RR4300/RR4314-1/RAND_RR4314-1.pdf
[7] Kranz, Ashley M., Teague Ruder, Ateev Mehrotra, and Andrew W. Mulcahy, Claims-Based
Reporting of Post-Operative Visits for Procedures with 10- or 90-Day Global Periods: Final
Report, Santa Monica, Calif.: RAND Corporation, RR-2846-CMS, 2019. As of October 15,
2019: https://www.rand.org/pubs/research_reports/RR2846.html
[8] Mulcahy, Andrew W., Harry H. Liu, Teague Ruder, Susan L. Lovejoy, Katie Merrell, and Ateev Mehrotra, Using Claims-Based Estimates of Post-Operative Visits to Revalue Procedures with 10- and 90-Day Global Periods, Santa Monica, Calif.: RAND Corporation, RR-3035-CMS, 2019. As of October 15, 2019: https://www.rand.org/pubs/research_reports/RR3035.html
[9] Gidengil, Courtney A., Andrew W. Mulcahy, Ateev Mehrotra, and Susan L. Lovejoy, Survey-Based Reporting of Post-Operative Visits for Select Procedures with 10- or 90-Day Global Periods: Final Report, Santa Monica, Calif.: RAND Corporation, RR-2941-CMS, 2019. As of October 15, 2019: https://www.rand.org/pubs/research_reports/RR2941.html
[10] p.8
[11] The notion that every service in the fee schedule has a value that is relative to all the other services in the fee schedule. This balance is overseen by the AMA-RUC, which makes recommendations to CMS on how to maintain relativity.
[12] Omnibus Budget Reconciliation Act (OBRA) of 1989 (P.L. 101-239)
[13] https://oig.hhs.gov/reports-and-publications/workplan/summary/wp-summary-0000309.asp
[14] Medicare and Medicaid Programs; CY 2025 Payment Policies under the Physician Fee Schedule and Other Changes to Part B Payment and Coverage Policies; Medicare Shared Savings Program Requirements; Medicare Prescription Drug Inflation Rebate Program (CMS-1807-P); Posted by the Centers for Medicare&Medicaid Services on Jul 10, 2024. p. 340. https://www.regulations.gov/document/CMS-2024-0256-0001
[15] CY 2025 PFS Proposed Rule, p. 342
[16] CY 2025 PFS Proposed Rule, p. 349
[17] CY 2025 PFS Proposed Rule, p. 1579
[18] CY 2025 PFS Proposed Rule, p. 352
[19] CY 2025 PFS Proposed Rule, pp. 353-4
[20] CY 2025 PFS Proposed Rule, p. 1580
Share via:

